Eczema (what to do if your child has eczema)
What is eczema and what causes it?
Eczema is a common long-term skin condition that causes the skin to be itchy, dry and red. It may start at any age but often in babies and can run in families.
Some children with eczema can also have asthma, hayfever and/or food allergies. The cause of eczema is complex but genes can play a part. A relative may have ‘atopy’ which is a tendency to eczema, asthma or hayfever. Allergy testing would identify food allergies if symptoms suggest this is necessary but would not show a cause for eczema.
How is eczema treated?
A child with eczema has a slightly faulty skin barrier, which lets water out and allows dust, irritants and bacteria in. Moisturiser (emollient) helps repair and protect the skin barrier. Redness caused by inflammation is treated with steroid creams (topical corticosteroids).
![]()
How do emollients work?
Emollients provide a coating on the skin which help the broken skin barrier and improve the level of moisture. A variety of different types can be used at different times of the day depending on the condition of your skin e.g. a cream may be preferred during the day with an ointment at night.
The vast majority of emollients can be used as a soap substitute. Regular soaps can be drying for skin and cause irritation.
Moisturisers (Emollients)
There are lots of different types of moisturisers;
- Gels – alcoholic or aqueous emulsion which liquefies on skin, often contain fragrances and preservatives.
- Lotions - contain oil and water, light to apply.
- Creams - water based, light, but contain preservatives so can sting especially if the child has very dry skin, also need to be applied frequently.
- Ointments – favored by dermatology as provide the best skin barrier, preservative free but thick and greasy. Not to be used if there is infection on the skin.
How much emollient is enough?
A thin shiny layer to the skin should be sufficient to all the affected areas. If treating the whole body approximately:
- 600g per week for an adult
- 250-500g per week for a child.
Top tips for emollients
- As a moisturiser
Smooth onto clean skin and apply as often as needed to prevent the skin becoming dry. Ideally it should be applied 2-4 times per day.
- As a cleanser
Apply liberally to the skin and wipe off with single layer of paper tissue, taking care not to damage fragile skin.
- As a soap substitute
Mix emollient with water in palm to form lather. Apply to the skin in a downwards direction. Gently rinse lather off skin leaving a thin layer of the ointment on the skin. Pat dry.
- In the bath
Ointments can be dissolved in water. Add a spoon full of ointment to a small amount of hot water in a jug. Then add to the bath water. Take care of the temperature of the water and when getting out of the bath, as it will be slippy.
How should emollients be applied?

Step 1
Always wash your hands for 20 seconds before applying a topical corticosteroid.

Step 2
Do not put your fingers into the tub as this can introduce bacteria and cause infection. Use a clean spoon or a spatula to take your emollient out of the tub.
If your emollient is in a pump this can be done straight on to your clean hands.

Step 3
Apply to the affected area in a downwards motion following the hair growth.
Do not rub in as this can block the follicles and cause infection.
What are topical corticosteroids?
Topical corticosteroids are a form of medicine applied directly to the skin which helps reduce inflammation, redness and irritation. The type of steroid is similar to those produced naturally in the body.
What are the different strengths of topical steroids?
Your doctor or specialist nurse will identify the correct strength of steroid for different parts of the body and discuss how to increase or decrease treatment appropriately using the steroid ladder.
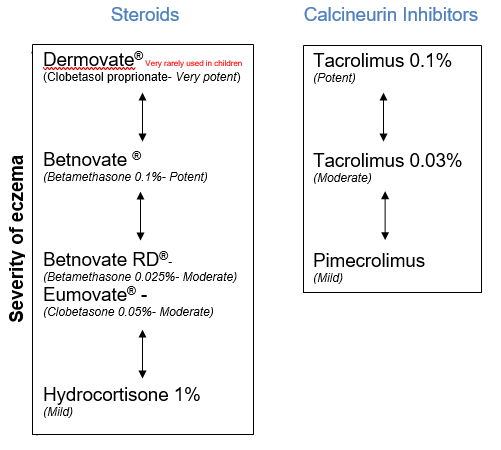
Topical corticosteroids are used on adults, children and young people. More potent steroids are typically in adults used on the affected areas on the body and mild/moderate steroids on the face and skin folds (under arms, breast folds, groin and genitals).
Children and young people will be guided by their doctor or specialist nurse with the use of mild and moderate steroids however when required potent steroids will be used when treating severe skin conditions.
How long should I use topical corticosteroids?
It is important that you follow the treatment plan given by your doctor or specialist nurse in order for your skin to avoid a flare of your skin condition. If used correctly topical corticosteroids should not cause side effects. Thinning of the skin and stretch marks will occur only if a strong steroid is used incorrectly or over a prolonged time.

Step 1
Always wash your hands for 20 seconds before applying a topical corticosteroid.

Step 2
Squeeze the topical steroid in a line from the last finger crease to the fingertip. This is a fingertip unit (FTU).
One FTU would be sufficient to treat an area equivalent to two adult handprints

Step 3
Apply to the affected area in a downwards motion following the hair growth.
Do not rub in as this can block the follicles and cause infection.
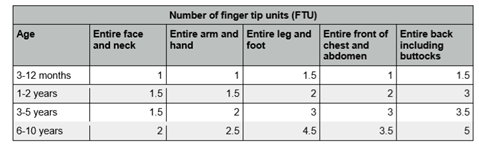
How much topical corticosteroid should be applied?
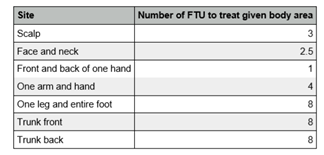
One (FTU) fingertip unit would be sufficient to treat an area equivalent to two adult handprints. In children the fingertip and two handprints are based on that of an adult also. A thin shiny layer should cover the affected area
The tables below show how much is estimated to be used. This is based on the whole area being treated therefore if only a proportion is affected the amount would be reduced.
Children
Adults and young people
Precautions
- Topical corticosteroids and emollients contain paraffin which is flammable. Do not smoke, use naked flames (e.g. candles, BBQs, lighters, cigarettes) whilst these products are in contact with your skin, clothes dressings or bandages.
- If a topical corticosteroid causes irritation, please seek advice from your medical or nursing team.
- An emollient should be applied at least 30 minutes after applying a topical steroid or vice versa.
- If you are having ultraviolet light treatment or radiotherapy, check with your medical and nursing team if there is any specific guidance on your emollient use prior to starting treatment.
- Topical corticosteroids and emollients do not contain SPF and should not be used as sun protection. Sun creams should be used when skin is exposed to direct sunlight with a medium/high UV level.
Wet wraps
Wet wrap bandages consist of two layers of medical grade viscose clothing or bandage. The first layer is applied wet and the second dry. Wet wraps help to moisten the skin and reduce irritation. Wet wraps can help intensify topical corticosteroid treatment. As the garment slowly dries out, the skin feels cooler which can help to reduce the itch sensation. Furthermore, they assist in breaking the itch-scratch cycle with eczema due to the barrier it provides in access to direct skin.
Common brands of garments / tubular bandage include Clinifast®, Comfifast®, Skinnies® and Tubifast®. The garments and tubular bandages come in different sizes to suit different aged children and large and small adults.
Paste bandages
Paste bandages are soaked in zinc oxide or zinc oxide plus ichthammol. These ingredients make the bandage soothing and cooling which helps to relive itching and soreness. Paste bandages have anti-inflammatory and anti-bacterial properties.
How do you apply paste bandages?
There is a special way to apply paste bandages because as they dry they can become tighter. Therefore, extra room is needed to make sure they remain comfortable. This technique should be demonstrated to you by a healthcare professional in the department.
Do not apply around the neck, face or torso to avoid suffocation.
Arm Application (National Eczema Society, 2018)
- Wash your hands.
- Open the pack and remove bandage.
- Start at the hand and work up the arm. Wrap the paste bandage around the wrist, smoothing it into place. After each turn, reverse the direction of the winding to form a pleat.
- Continue up the arm and over the elbow, smoothing the paste bandage into place and reversing the direction of the winding (clockwise/anticlockwise) with each turn to make a pleat.
- Secure the paste bandage in place with a dry bandage, such as CLINI fast Tubular Bandage.
- If the fingers are affected, small strips of paste bandage can be wrapped around individual digits and moulded for comfort.
Patch Application
- Wash your hands.
- Open the pack and remove bandage.
- Cut an appropriate size patch and apply directed to the skin.
- Secure in place with dry bandage, such as CLINI fast Tubular Bandage. Alternatively secure in place with Cotton Garments.
Leg Application (National Eczema Society, 2018)
- Wash your hands.
- Open the pack and remove bandage.
- Start at the base of the toes and wrap paste bandage around the ball of the foot or heel, smoothing it into place. After each turn, reverse the direction of the winding to form a pleat.
- Continue up the lower leg and over the knee to the top of the leg, smoothing the paste bandage into place and reversing the direction of the winding (clockwise/anticlockwise) with each turn to make a pleat.
- Secure the paste bandage in place with a dry bandage, such as CLINI fast Tubular Bandage.
- If the toes are affected, small strips of paste bandage can be wrapped around individual digits and moulded for comfort.
What are the possible side effects of paste bandages?
Commonly paste bandages are used with topical corticosteroids underneath which increases the strength of them. A healthcare professional should always discuss your treatment plan with you before using paste bandages and topical corticosteroids together.
Environmental Triggers
Skin conditions can be triggered by many environmental irritants which include house dust mite, pets, pollen, moulds, central heating, laundry and cleaning products. It is impossible to eliminate all triggers but you can minimise these with some simple measures.
How to reduce house dust mites?
House dust mites are one of the biggest triggers in eczema and other skin conditions. They are tiny insects that feed skin we shed and are found in soft furnishings.
- You can reduce the amount of dust mites in your home by: vacuuming carpets regularly- daily if possible.
- Vacuum mattresses, pillows and covers at least twice a week. Damp dust surfaces and floors on a regular basis.
- Avoid dry dusting, as this can spread dust into the air.
- Wash bed linen weekly on high temperature and wash curtains every 2-3 months.
- Limit soft toys, have one special soft toy in the bed and wash this regularly on a high temperature or put in a plastic bag in the freezer overnight to kill off the dust mites.
How to reduce irritation by pets?
It's not pet fur that causes an allergic reaction but its flakes of their skin, saliva and dried urine. It may not be possible to remove a pet permanently but you could try:
- Keeping pets outside the house as much as possible.
- Not allowing pets into bedrooms.
- Washing pets regularly.
- Opening windows to increase ventilation.
How to reduce the impact of pollen?
Pollen allergy / hay fever is triggered when trees and grasses release pollen into the air. Typically, people are affected during spring (trees) and summer (grasses).
To help keep this under control you could:
- Avoid drying clothes outside when pollen count is high.
- Keep doors and windows shut where possible.
- Shower and change clothes from being outside.
- Avoid grassy areas, such as parks and fields, particularly in the early morning, evening or night, when the pollen count is highest.
How to reduce mould?
Tiny particles released by moulds can also cause an allergic reaction in some people. You can prevent this by:
- Dealing with any damp and condensation in your home.
- Keeping your home dry and well ventilated.
- Not storing clothes in damp cupboards.
- Removing any indoor pot plants from your home.
How to reduce the impact of central heating?
Central heating reduces humidity and dries the skin, making it itchy. You could control this by: Keeping your house at a comfortable 18°c. Hydrate your skin by applying moisturisers or emollient often when in the house
How to reduce the impact of laundry and cleaning products?
People with eczema should take special care with the items that come into direct contact with their skin. For most people fragrances (perfumes) and detergents are what cause skin reactions. Air fresheners, candles, wax melts and diffusers are also irritants and use should be avoided.
To help keep this under control you could: Use non bio washing powder when washing clothes. Use your washing machine’s second or “extra rinse” setting if it has one. Do not use fabric conditioner.