FASD what is it?
Fetal Alcohol Spectrum Disorder (FASD) for young people
FASD is a life changing and life long condition. It is surprisingly common. It is caused by drinking alcohol during pregnancy.
Many women don’t realise they are pregnant during the first few weeks or didn’t plan to get pregnant.
Most people in the UK aren’t aware of the severe harm that drinking alcohol in pregnancy can cause to the unborn baby.
Studies suggest FASD affects at least 3.6% of the UK population (McCarthy et al, 2021, McQuire et al 2019). This means that 1 child in every classroom is likely to be affected by FASD.
When a pregnant woman drinks any alcohol
The alcohol in the bloodstream crosses the placenta and affects the baby.
Doctors and midwives agree that drinking alcohol in pregnancy increases the chances of miscarriage, premature birth and still birth. Even after a safe delivery, the chances of cot death maybe increased (officially known as Sudden Infant Death Syndrome or SIDS).
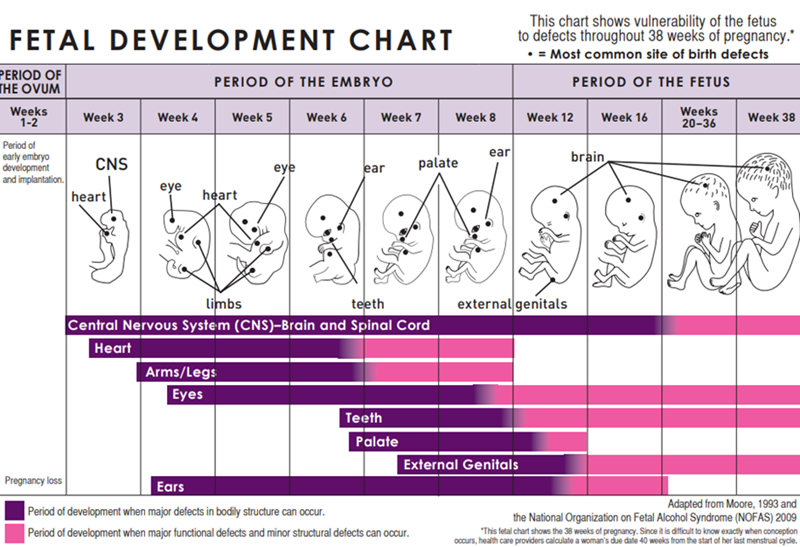
The unborn baby does not have a mature liver to process and detoxify alcohol. The human brain develops throughout everyday of the pregnancy. The harm caused to the baby depends on the organs and brain development happening at the time the alcohol is consumed.
FASD is preventable!

If you have been drinking alcohol and have found that you are pregnant please speak to your midwife to get support and advice.
The Chief Medical Officers' guideline is that: If you are pregnant or planning a pregnancy, the safest approach is not to drink alcohol at all, to keep risks to your baby to a minimum.
Remember no alcohol no risk!
There is no safe time and no safe amount to drink during pregnancy as alcohol can harm the baby throughout.
FASD is a spectrum disorder. This means that everyone who has FASD may display the symptoms in different ways.
Less than 10% of people with FASD will have facial characteristics. This is because the face only develops in very early pregnancy.
In many cases FASD goes undiagnosed and is a hidden disability. The cause of behaviours and difficulties may be misundertood.
Individuals with FASD can have over 400 possible symptoms including behaviours that are common in ADHD and Autism. These may include:
- Physical health problems affecting any part of the body.
- Severe difficulties with movement and co-ordination
- Problems understanding instructions
- Struggle with friendships and social interactions
- Difficulties in school and work environment
- Find it challenging to concentrate and focus
- Impulsive behaviours and difficulty managing these
- Poor comprehension of social rules and expectation
- Difficulty organising themselves in daily life
- Hyperactivity
- Easily overwhelmed and over stimulated
- Poor sleep
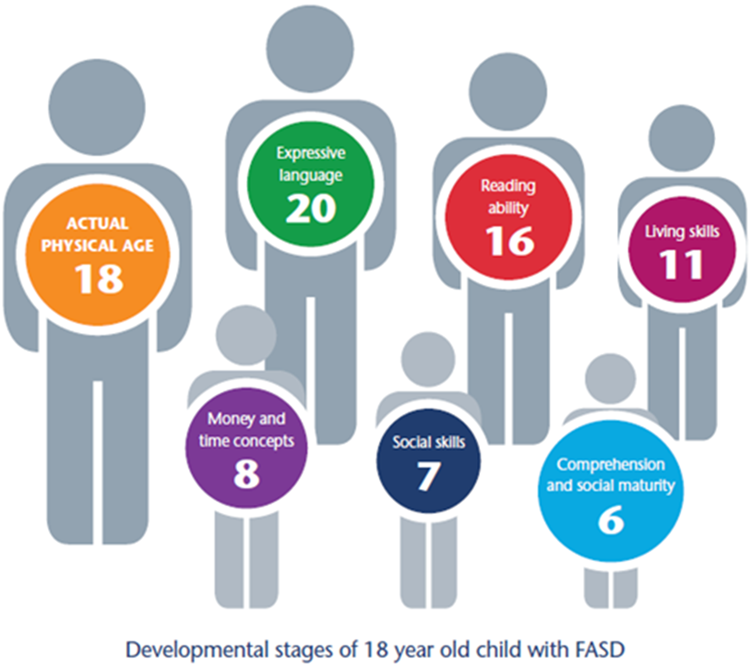
An 18 year old person with FASD may look like anyone else of their age but their skills and abilities may vary from their friends who do not have FASD.
They may act in ways that are more typical of a child half their age. Coping with daily life and making friends can be very challenging. Individuals with FASD are often vulnerable to exploitation.
The good news
Children and adults living with FASD can live happy and productive lives if their FASD is identified early and they get the right support.
People with FASD can have many skills and talents and may excel in sport, music or the arts.
If a child needs extra help because of FASD they might be identified as having a Special Educational Need or Disability. More information is available about this support search your area's SEND local offer.
If you are concerned that a child might be impacted by FASD
Speak to your GP, Health Visitor, School SENCO or School Nurse.
Spread the word!
We all need to raise awareness of FASD and the risks of alcohol harms in pregnancy.
Useful resources
References
McCarthy R, Mukherjee RAS, Fleming KM, etal. Prevalence of fetal alcohol spectrum disorder in Greater Manchester, UK: An active case ascertainment study. Alcohol Clin Exp Res 2021. . doi: 10.1111/acer.14705 pmid: 34590329
McQuire C, Mukherjee R, Hurt L, etal. Screening prevalence of fetal alcohol spectrum disorders in a region of the United Kingdom: A population-based birth-cohort study. Prev Med 2019;118:344-51. doi: 10.1016/j.ypmed.2018.10.013 pmid: 30503408
Schölin, L., Mukherjee, R., Aiton, N., Blackburn, C., Brown, S., Flemming, K., Gard, P., Howlett, H., Plant, M., Price, A., Shields, J., Smith, L., Suttie, M., Zammitt, D. & Cook, P., (2021) Fetal alcohol spectrum disorders: an overview of current evidence and activities in the UK. Archives of Disease in Childhood, Archives of disease in childhood, 2021-01-13. http://dx.doi.org/10.1136/archdischild-2020- 319572
Pages in this section
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor.
- If your child has any of the above features, urgently see your GP. For an urgent out-of-hours GP appointment, call NHS 111.
- You should only call 999 or go to your nearest A&E department in critical or life threatening situations.
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP.
- Remember that if your child's condition gets worse, you should seek further medical advice immediately.
- Help your child to understand - watch this video with them about going to the pharmacy.
For information on common childhood illnesses go to What is wrong with my child?
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP.
- Remember that if your child's condition gets worse, you should seek further medical advice immediately.
- Help your child to understand - watch this video with them about going to the pharmacy.
For information on common childhood illnesses go to What is wrong with my child?
Health visitors are nurses or midwives who are passionate about promoting healthy lifestyles and preventing illness through the delivery of the Healthy Child Programme. They work with you through your pregnancy up until your child is ready to start school.
Health Visitors can also make referrals for you to other health professionals for example hearing or vision concerns or to the Community Paediatricians or to the child and adolescent mental health services.
Contact them by phoning your Health Visitor Team or local Children’s Centre.
Sound advice
Health visitors also provide advice, support and guidance in caring for your child, including:
- Breastfeeding, weaning and healthy eating
- Exercise, hygiene and safety
- Your child’s growth and development
- Emotional health and wellbeing, including postnatal depression
- Safety in the home
- Stopping smoking
- Contraception and sexual health
- Sleep and behaviour management (including temper tantrums!)
- Toilet training
- Minor illnesses
For more information watch the video: What does a health visitor do?
Health visitors are nurses or midwives who are passionate about promoting healthy lifestyles and preventing illness through the delivery of the Healthy Child Programme. They work with you through your pregnancy up until your child is ready to start school.
Health Visitors can also make referrals for you to other health professionals for example hearing or vision concerns or to the Community Paediatricians or to the child and adolescent mental health services.
Contact them by phoning your Health Visitor Team or local Children’s Centre.
Sound advice
Health visitors also provide advice, support and guidance in caring for your child, including:
- Breastfeeding, weaning and healthy eating
- Exercise, hygiene and safety
- Your child’s growth and development
- Emotional health and wellbeing, including postnatal depression
- Safety in the home
- Stopping smoking
- Contraception and sexual health
- Sleep and behaviour management (including temper tantrums!)
- Toilet training
- Minor illnesses
For more information watch the video: What does a health visitor do?
Midwives provide advice, care and support for women and their babies during pregnancy, labour and the early postnatal period. They provide health education and parenting advice until care is transferred to a health visitor. This usually happens when your baby is about 2 weeks old.
Sound Advice
A midwife is an expert in normal pregnancy and birth.
Midwives provide advice, care and support for women and their babies during pregnancy, labour and the early postnatal period. They provide health education and parenting advice until care is transferred to a health visitor. This usually happens when your baby is about 2 weeks old.
Sound Advice
A midwife is an expert in normal pregnancy and birth.
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors/GPs can treat many illnesses that do not warrant a visit to A&E.
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors/GPs can treat many illnesses that do not warrant a visit to A&E.
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, call 111. An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services.
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, call 111. An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services.
For information on common childhood illnesses go to What is wrong with my child?
A&E departments provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.
Sound advice
A&E departments provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.
Sound advice
School nurses care for children and young people, aged 5-19, and their families, to ensure their health needs are supported within their school and community. They work closely with education staff and other agencies to support parents, carers and the children and young people, with physical and/or emotional health needs.
Contacting the School Nurse
Primary and secondary schools have an allocated school nurse – telephone your child’s school to ask for the contact details of your named school nurse.
There is also a specialist nurse who works with families who choose to educate their children at home.
Sound Advice
Before your child starts school your health visitor will meet with the school nursing team to transfer their care to the school nursing service. The school nursing team consists of a school nursing lead, specialist public health practitioners and school health staff nurses.
They all have a role in preventing disease and promoting health and wellbeing, by:-
- encouraging healthier lifestyles
- offering immunisations
- giving information, advice and support to children, young people and their families
- supporting children with complex health needs
Each member of the team has links with many other professionals who also work with children including community paediatricians, child and adolescent mental health teams, health visitors and speech and language therapists. The school health nursing service also forms part of the multi-agency services for children, young people and families where there are child protection or safeguarding issues.
School nurses care for children and young people, aged 5-19, and their families, to ensure their health needs are supported within their school and community. They work closely with education staff and other agencies to support parents, carers and the children and young people, with physical and/or emotional health needs.
Contacting the School Nurse
Primary and secondary schools have an allocated school nurse – telephone your child’s school to ask for the contact details of your named school nurse.
There is also a specialist nurse who works with families who choose to educate their children at home.
Sound Advice
Before your child starts school your health visitor will meet with the school nursing team to transfer their care to the school nursing service. The school nursing team consists of a school nursing lead, specialist public health practitioners and school health staff nurses.
They all have a role in preventing disease and promoting health and wellbeing, by:-
- encouraging healthier lifestyles
- offering immunisations
- giving information, advice and support to children, young people and their families
- supporting children with complex health needs
Each member of the team has links with many other professionals who also work with children including community paediatricians, child and adolescent mental health teams, health visitors and speech and language therapists. The school health nursing service also forms part of the multi-agency services for children, young people and families where there are child protection or safeguarding issues.