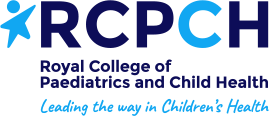
Signs of an asthma attack include:
- Sounding very wheezy
- Having a tight chest
- Finding it hard to breath
- Being too breathless to talk or walk.
Sometimes there is no obvious cause for your child’s asthma attack. The most common triggers are viral infections (coughs, colds and chest infections), emotional anxiety and exposure to airway irritants such as cigarette smoke.
What should I do if my child is having an asthma attack?
- Sit your child upright
- Keep them calm and reassure them
- Refer to your child’s action plan and follow the instructions.
For more information on how to beat asthma please visit the Beat Asthma website
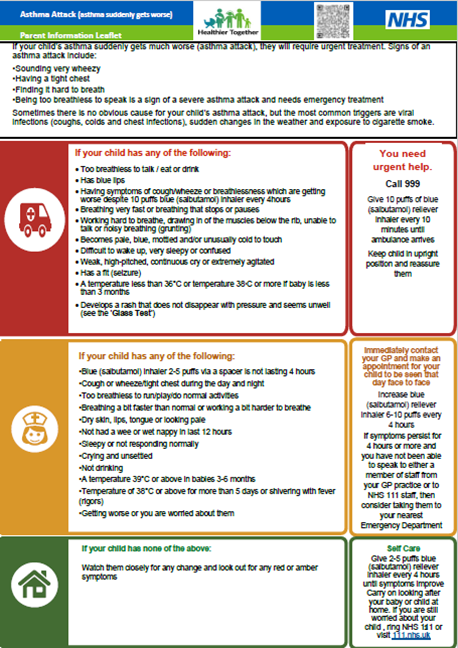
Asthma attack (asthma suddenly gets worse)
This guidance has been reviewed and adapted by healthcare professionals across North East and North Cumbria with consent from the Hampshire development groups.
This guidance is written by healthcare professionals from across Hampshire, Dorset and the Isle of Wight.
Asthma attack prevention
The most common triggers are viral infections, emotional disturbance and exposure to airway irritants such as cigarette smoke.
Things you can do to reduce the chance of your child having an asthma attack: Get your child’s asthma under control
1. Get your child’s asthma under control
Children with poorly controlled asthma are much more likely to have an asthma attack. Make sure your child follows their action plan.
Signs of poorly controlled asthma:
- Needing additional doses of inhaler 3 or more times a week
- Wheezy after exercise
- Persistent night-time cough
If your child has symptoms of poorly controlled asthma they should be reviewed. Make an appointment with their GP or asthma nurse.
It is important to have a yearly asthma review with your asthma nurse or GP. Everyone with asthma should have an action plan.
2. Get the inhaler technique right
Watch these Beat Asthma videos on how to help your child use their inhaler.
Your child’s asthma will not be controlled if their medicines are not getting into their lungs.
If your child has been given a spacer:
- Check the inhaler contains medicine and shake. Reliever inhalers have a maximum of 200 doses but will continue to fire when empty.
- Remove the cap.
- Fit the inhaler into the end of the spacer.
- For spacer with mask, place the mask over the nose and mouth and ensure a good seal. For spacer and mouthpiece, place teeth around the mouthpiece and seal with lips. Most children over 3 years can use a mouthpiece.
- Press the inhaler once and encourage the child to take 5 slow breaths or count to 10 slowly whilst they breath normally through the spacer.
- Shake the inhaler and repeat steps 4 and 5 if more puffs are needed.
See your practice nurse or doctor if you are not sure whether your child is using their inhaler properly.
3. Avoid triggers where possible
Even when adults smoke away from their children, smoke on their clothes and hair can make their child’s asthma worse.
If needed visit the your local stop smoking site.
4. Your child should have an influenza immunisation every autumn (the flu jab)
Flu viruses can trigger asthma symptoms. Current guidelines in the UK recommend that high-risk groups such as people with severe asthma should have a flu jab each winter.