Infant Head Shape Abnormalities
Overview
- Head shape abnormalities are common - present in 25% of infants aged under 6 months
- Deformational posterior plagiocephaly accounts for the vast majority of cases
- Craniosynostosis (early fusion of cranial sutures) is rare
- Clinical examination alone is sufficient to differentiate between deformational plagiocephaly and craniosynostosis in 95% of cases, imaging may be required in the remainder
- Deformational plagiocephaly resolves spontaneously, but may take 2-3 years for complete resolution
Clinical approach
- Measure and plot orbitofrontal circumference (OFC)
- Assess overall muscle tone
- Observe the head from above:
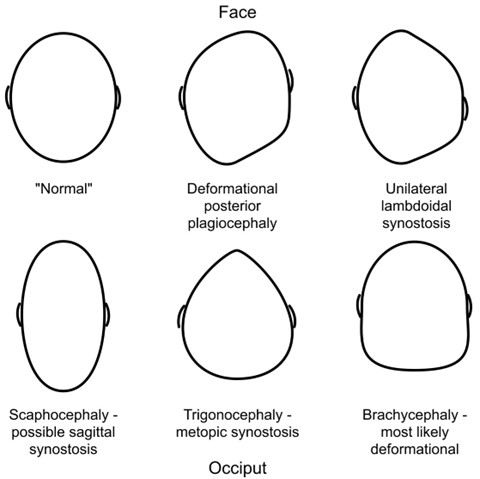
Asymmetrical occipital flattening (the most common reason for seeking advice)
- In deformational posterior plagiocephaly, the head will appear flattened to one side of the occiput and the ear on the ipsilateral side will appear to be displaced anteriorly compared to the contralateral ear. If there is accompanying anterior asymmetry, the forehead will be prominent on the ipsilateral side.
- In unilateral lambdoidal craniosynostosis, the ear on the ipsilateral side will appear to be displaced posteriorly compared with the contralateral ear. If there is accompanying anterior asymmetry, the forehead will be prominent on the contralateral side. In addition, when viewed from the back of the head, the ear on the flattened side will appear to be displaced inferiorly.
Ridging of sutures
- Ridging most commonly occurs in the metopic suture. In the absence of an abnormal head shape (typically a reduction in bitemporal diameter resulting in trigonocephaly)
- Ridging may also be seen in the sagittal suture; this is indicative of sagittal craniosynostosis and occurs as a result of peri-sutural osteosclerosis and is detectable from very early infancy
- Ridging may sometimes be mistaken for overlapping sutures. This may be occur as a result of cranial moulding during delivery and will resolve in first days of life or as a result of microcephaly – measurement of OFC will identify this.
Examine for torticollis, which may contribute to deformational plagiocephaly
Management
Suspected craniosynostosis should be referred to a general paediatric clinic for confirmation and subsequent referral to a supraregional craniofacial unit
Active repositioning for plagiocephaly should be explained – wait until the child is asleep and then reposition the head
Helmets are not available on the NHS – it is likely that they improve appearances more quickly than active repositioning alone but the final cosmetic results are likely to be equal
Children with torticollis should be referred for physiotherapy
Red flags
- OFC crossing through centiles – refer to general paediatrics
- Poor muscle tone – plagiocephaly may be the first sign of neurodevelopmental problems – refer for further assessment to general or community paediatrics
Patient information: Plagiocephaly and brachycephaly (flat head syndrome) - NHS (www.nhs.uk)
Pages in this section
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor.
- If your child has any of the above features, urgently see your GP. For an urgent out-of-hours GP appointment, call NHS 111.
- You should only call 999 or go to your nearest A&E department in critical or life threatening situations.
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP.
- Remember that if your child's condition gets worse, you should seek further medical advice immediately.
- Help your child to understand - watch this video with them about going to the pharmacy.
For information on common childhood illnesses go to What is wrong with my child?
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP.
- Remember that if your child's condition gets worse, you should seek further medical advice immediately.
- Help your child to understand - watch this video with them about going to the pharmacy.
For information on common childhood illnesses go to What is wrong with my child?
Health visitors are nurses or midwives who are passionate about promoting healthy lifestyles and preventing illness through the delivery of the Healthy Child Programme. They work with you through your pregnancy up until your child is ready to start school.
Health Visitors can also make referrals for you to other health professionals for example hearing or vision concerns or to the Community Paediatricians or to the child and adolescent mental health services.
Contact them by phoning your Health Visitor Team or local Children’s Centre.
Sound advice
Health visitors also provide advice, support and guidance in caring for your child, including:
- Breastfeeding, weaning and healthy eating
- Exercise, hygiene and safety
- Your child’s growth and development
- Emotional health and wellbeing, including postnatal depression
- Safety in the home
- Stopping smoking
- Contraception and sexual health
- Sleep and behaviour management (including temper tantrums!)
- Toilet training
- Minor illnesses
For more information watch the video: What does a health visitor do?
Health visitors are nurses or midwives who are passionate about promoting healthy lifestyles and preventing illness through the delivery of the Healthy Child Programme. They work with you through your pregnancy up until your child is ready to start school.
Health Visitors can also make referrals for you to other health professionals for example hearing or vision concerns or to the Community Paediatricians or to the child and adolescent mental health services.
Contact them by phoning your Health Visitor Team or local Children’s Centre.
Sound advice
Health visitors also provide advice, support and guidance in caring for your child, including:
- Breastfeeding, weaning and healthy eating
- Exercise, hygiene and safety
- Your child’s growth and development
- Emotional health and wellbeing, including postnatal depression
- Safety in the home
- Stopping smoking
- Contraception and sexual health
- Sleep and behaviour management (including temper tantrums!)
- Toilet training
- Minor illnesses
For more information watch the video: What does a health visitor do?
Midwives provide advice, care and support for women and their babies during pregnancy, labour and the early postnatal period. They provide health education and parenting advice until care is transferred to a health visitor. This usually happens when your baby is about 2 weeks old.
Sound Advice
A midwife is an expert in normal pregnancy and birth.
Midwives provide advice, care and support for women and their babies during pregnancy, labour and the early postnatal period. They provide health education and parenting advice until care is transferred to a health visitor. This usually happens when your baby is about 2 weeks old.
Sound Advice
A midwife is an expert in normal pregnancy and birth.
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors/GPs can treat many illnesses that do not warrant a visit to A&E.
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors/GPs can treat many illnesses that do not warrant a visit to A&E.
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, call 111. An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services.
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, call 111. An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services.
For information on common childhood illnesses go to What is wrong with my child?
A&E departments provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.
Sound advice
A&E departments provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.
Sound advice
School nurses care for children and young people, aged 5-19, and their families, to ensure their health needs are supported within their school and community. They work closely with education staff and other agencies to support parents, carers and the children and young people, with physical and/or emotional health needs.
Contacting the School Nurse
Primary and secondary schools have an allocated school nurse – telephone your child’s school to ask for the contact details of your named school nurse.
There is also a specialist nurse who works with families who choose to educate their children at home.
Sound Advice
Before your child starts school your health visitor will meet with the school nursing team to transfer their care to the school nursing service. The school nursing team consists of a school nursing lead, specialist public health practitioners and school health staff nurses.
They all have a role in preventing disease and promoting health and wellbeing, by:-
- encouraging healthier lifestyles
- offering immunisations
- giving information, advice and support to children, young people and their families
- supporting children with complex health needs
Each member of the team has links with many other professionals who also work with children including community paediatricians, child and adolescent mental health teams, health visitors and speech and language therapists. The school health nursing service also forms part of the multi-agency services for children, young people and families where there are child protection or safeguarding issues.
School nurses care for children and young people, aged 5-19, and their families, to ensure their health needs are supported within their school and community. They work closely with education staff and other agencies to support parents, carers and the children and young people, with physical and/or emotional health needs.
Contacting the School Nurse
Primary and secondary schools have an allocated school nurse – telephone your child’s school to ask for the contact details of your named school nurse.
There is also a specialist nurse who works with families who choose to educate their children at home.
Sound Advice
Before your child starts school your health visitor will meet with the school nursing team to transfer their care to the school nursing service. The school nursing team consists of a school nursing lead, specialist public health practitioners and school health staff nurses.
They all have a role in preventing disease and promoting health and wellbeing, by:-
- encouraging healthier lifestyles
- offering immunisations
- giving information, advice and support to children, young people and their families
- supporting children with complex health needs
Each member of the team has links with many other professionals who also work with children including community paediatricians, child and adolescent mental health teams, health visitors and speech and language therapists. The school health nursing service also forms part of the multi-agency services for children, young people and families where there are child protection or safeguarding issues.