Transition from children's to adult healthcare - for professionals

The transition from paediatric to adult services can be a frightening and confusing time for young people, their families and carers. Paediatric teams often have more flexibility and are able to take an holistic, whole person approach rather than a condition or organ specific focus. The new clinical teams often don’t have in-depth knowledge of a young person’s complex condition. It can also cause considerable workload, headaches and last-minute panic for the primary care team when services that have been in place for years are suddenly not available anymore. This is particularly true for young people with life limiting and complex conditions, who are often the most vulnerable.
Transition and transfer of care
There is a growing body of evidence supporting and informing best practice in relation to the transition and transfer of care.
Research from Northumbria University highlighted that during transition from children's to adult healthcare, young adults with long-term conditions may show delays in psychosocial development compared to their peers without long-term conditions, and deterioration of their conditions’ medical control. The impact of this is increased non-elective admissions, more frequent medical emergencies, reduced medication compliance and poorer health outcomes.
The research found three features of transitional healthcare were associated with improved outcomes:
- appropriate parent/carer involvement
- promotion of young people's confidence in managing their health
- meeting the adult team before transfer
NICE have produced standards and guidance on transition and transfer to adult health services.
The preparation of a patient and their family for transfer to adult services is referred to as transition. The timing of transfer to adult services depends on patient preparedness. Most patients will move to adult services between their 16th and 19th birthday. Some young people will be ready to move to adult services at 16 years others may need extra support and time.
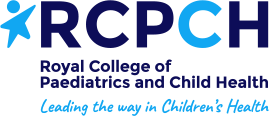
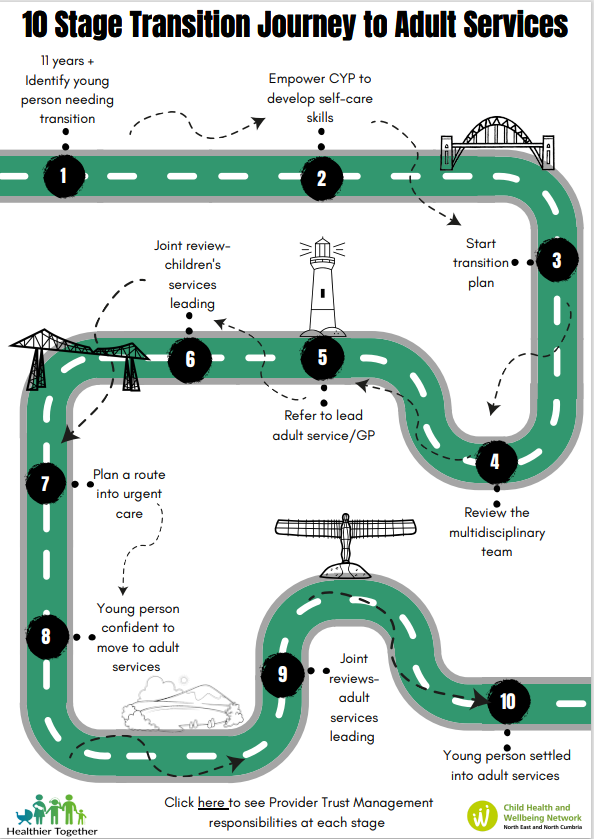
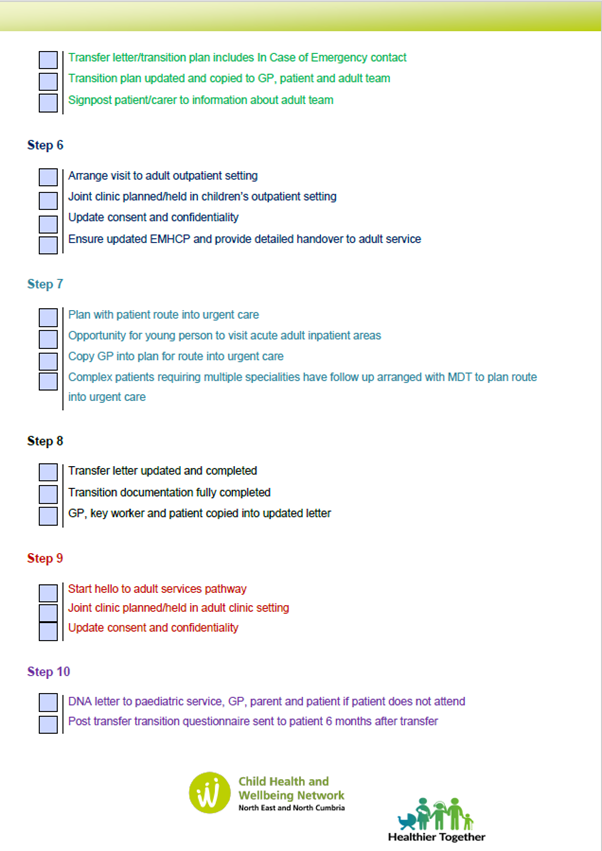
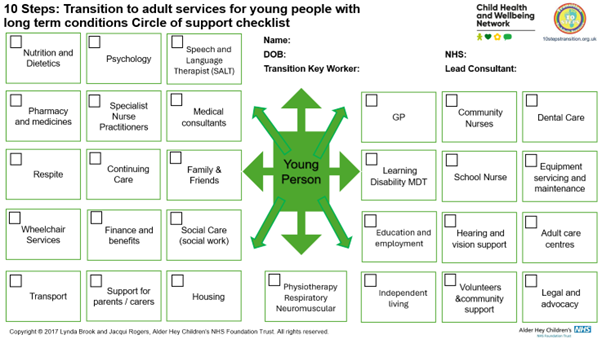
All professionals should strive to provide developmentally appropriate healthcare Northumbria toolkit up to aged 25 years. To assist with this the North East and North Cumbria (NENC) Transitions Regional Core Steering Group have developed an aspirational transition pathway known as the 'Journey to Adult Healthcare'. The NENC 10 Stage Transition Journey builds on the work of the North West Transition Network and Alder Hey NHS FT and is based on the 10 Steps to Transition Framework, with their support and permission.
For more information on the Northumbria University Developmentally Appropriate Healthcare full study, please see facilitating transition of young people with long-term health conditions
Although the transition process needs to be tailored to the specific needs of an individual young person, the core elements remain the same. A number of different guidelines and pathways have been developed to inform flexible and adaptable models of care designed to meet the needs of individual young people and their families.
A 2020 North-East and North Cumbria regional survey led by the Child Health and Wellbeing Network identified pockets of excellent practice and a willingness amongst both paediatric and adult professionals to further develop their approach to transition.
Transitions DAH Findings and Recommendations Report
The following pathways have been developed to help professionals support young people and parents/carers as they move through the transition process.

For more information on the Northumbria University Developmentally Appropriate Healthcare full study, please see facilitating transition of young people with long-term health conditions
Although the transition process needs to be tailored to the specific needs of an individual young person, the core elements remain the same. A number of different guidelines and pathways have been developed to inform flexible and adaptable models of care designed to meet the needs of individual young people and their families.
A 2020 North-East and North Cumbria regional survey led by the Child Health and Wellbeing Network identified pockets of excellent practice and a willingness amongst both paediatric and adult professionals to further develop their approach to transition.
Transitions DAH Findings and Recommendations Report
The following pathways have been developed to help professionals support young people and parents/carers as they move through the transition process.

Transition toolkit
Further work has been done to enhance the regional aspirational pathway in consideration of the elevated needs of people with complex needs. This work has been led by a working group of the North East & North Cumbria Regional Core Steering Group.
Things to think about
Questions you could be asked by the young people, which you should be prepared to answer:
- What is the plan for my transition?
- When am I moving to adult services?
- Can I choose which adult service I move to?
- What is different about the adult service?
- Who do I contact if I am unwell? Where will I be admitted?
- Can I meet the adult staff before I leave children’s services?
- Can I visit the adult service to look around?
- Are there any young people I can talk to about moving to adult services?
- What do I need to know before I move to the adult service?
- When can I start getting more involved in my health care?
- How will my condition affect my future, such as my education and employment prospects?
The Ask 3 Questions campaign was designed to help patients access useful information about their condition.
By talking about transition early, young people should have plenty of time for discussions and their questions, ensuring that they are fully prepared when the time comes to make the move to adult services.
The healthcare team should be supportive in discussing the process of transition with the young people.

Together for Short Lives webinar
This webinar, hosted by Royal College of General Practitioners and ‘Together for Short Lives’ introduces new eLearning and discusses how to improve the transition journey for young people and their families with the help of the general practice team, resulting in a more streamlined workload for primary care teams and a better experience for their patients.
A parent's experience
Lottie's mum shares her experience
Christie, Lottie's mum shares their experience of transition. She gives some useful tips and advice on how things could have been improved for Lottie.
Thank you to Christie and Lottie for sharing their story and for the support to make this available to others via the Healthier Together platform.
Mental Capacity and Decision Making
 All care decisions must come from a shared partnership between the professional and the child, young person or adult. But for those who do not have capacity for their choices, or may lose that capacity in the future it is important that the right choices are made. As a healthcare professional you have a responsibility to encourage, support and facilitate a young person's participation in decision making and uphold their rights under the Mental Capacity Act (MCA) 2005. Mencap have developed a useful set of resources around mental capacity.
All care decisions must come from a shared partnership between the professional and the child, young person or adult. But for those who do not have capacity for their choices, or may lose that capacity in the future it is important that the right choices are made. As a healthcare professional you have a responsibility to encourage, support and facilitate a young person's participation in decision making and uphold their rights under the Mental Capacity Act (MCA) 2005. Mencap have developed a useful set of resources around mental capacity.
For individuals who lack capacity to engage independently in the completion of an Advance Statement or Advance Decision to Refuse Treatment (ADRT) conversations are necessary regarding any known preferences and wishes and estimating what the person would want should be discussed between their relatives, carers and health professionals. This should be done via the best decision making process in line with MCA 2005. The agreed information should then be documented in a clear format and supported by MCA best interest decision making documentation
For more information and supporting resources and form templates about Advance Care Planning and Deciding Right please see Deciding Right Resources - Northern Cancer Alliance Northern Cancer Alliance
Gillick competency and Fraser guidelines
Gillick competency and Fraser guidelines help people who work with children to balance the need to listen to children's wishes with the responsibility to keep them safe. When practitioners are trying to decide whether a child is mature enough to make decisions about things that affect them, they often talk about whether the child is 'Gillick competent' or whether they meet the 'Fraser guidelines'. The Fraser guidelines still apply to advice and treatment relating to contraception and sexual health but the Gillick competency is often used in a wider context to help assess whether a child has the maturity to make their own decisions and to understand the implications of those decisions.
Professionals should always encourage a child to tell their parents or carers about the decisions they are making. If young people don't want to do this, you should explore why and, if appropriate, discuss ways to help them inform their parents or carers. More information is available on the NSPCC website (Gillick competence and Fraser guidelines | NSPCC Learning)